The Great Cellular Heist: H5N1 Adapts for a Human Host
New research offers implications for a vaccine to combat avian flu
By Anna Holt
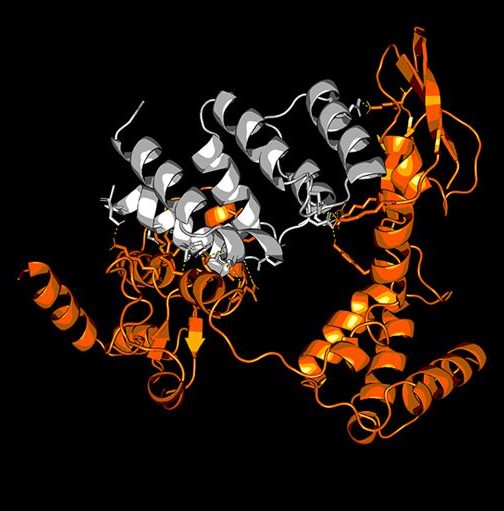
A 3-D model of two proteins, Polymerase Basic 2 (in orange) and Mitochondrial Antiviral Signaling (in grey), interacting. PB2 is a part of the Influenza virus, while MAVS is a protein in human cells that is part of the innate immune system cells use to fight infections. In recent strains of H5N1 influenza, Charlotte researchers measured a trend of increasing strength of interaction between these two proteins and concluded that H5N1 Influenza is beginning to overcome human cells’ ability to fight the infection.
H5N1 is no longer just a threat to poultry farms. It’s a fast-evolving virus with a growing ability to infect mammals — including cows and humans — and scientists at UNC Charlotte have the data to prove it.
Recent findings by genomics and bioinformatics researchers in the Center for Computational Intelligence to Predict Health and Environmental Risks documents key mutations that help the virus hijack human cells by blocking immune defenses. This indicates the risk to human health is expected to rise as H5N1 evolves to better infect mammals.
This rapid adaptation means that “an H5N1 vaccine made for an earlier strain will have less efficacy,” said Colby T. Ford,’14,’15 M.S.,’18 Ph.D., now a CIPHER visiting scholar in data science.
The UNC Charlotte research will prove pivotal (as did a similar studies* by the same group on COVID-19 mutations) as global leaders weigh the public health response to avian influenza.
“We are entering a whole new era of molecular epidemiology in which we provide functional insights above and beyond disease surveillance.”
Daniel Janies, Ph.D., CIPHER co-director and the Carol Grotnes Belk Distinguished Professor in Bioinformatics and Genomics

While many refer to the virus as simply “bird flu,” scientists have long surveilled avian influenza to find it is indeed a zoonotic virus — meaning it can and does hop from birds to mammals, such as cows and humans. UNC Charlotte’s research indicates current lineages of the virus are equally able to infect bird and mammal cells.
In fact, the most recent H5N1 strains show signs of the virus being able to replicate itself much more readily in mammals than previously known. The most up-to-date research from the team at UNC Charlotte documents H5N1’s “strengthening immune evasion capabilities.”
In a March 17 preprint manuscript, for which peer-review is underway, researchers explain that at least two genes of the virus have changed over time — allowing avian influenza to improve its ability to hijack mammalian cells.
Takeaways: CIPHER’s H5N1 Research
- The H5N1 strain of the Influenza A virus is changing rapidly, evading typical immunological defenses
- H5N1 is already a pandemic among nearly 250 species of wild and domestic birds and mammals in North America, including chickens and cows
- As the virus evolves, risk to human health grows
- The efficacy of the current vaccine – due to H5N1’s ability to change – is decreasing
- The food supply for humans is safe – but poultry and eggs should be cooked to an internal temperature of 165 degrees and only dairy products that are pasteurized should be consumed. For pet food, pay attention to recalls for brands contaminated with avian influenza.
While avian influenza has yet to achieve human-to-human transmission, it is already considered a pandemic among animals.
The virus has infected small mammals and hundreds of species of wild and domestic birds, and in recent years, H5N1 has expanded its reach to larger mammals, including cattle. This change in host range significantly increases the risk of human infection, particularly as the virus evolves to evade immune defenses.
As Ford explains, the weakening of antibody binding affinity to newer viral strains means that we could be facing an H5N1 strain capable of efficiently infecting humans, with potentially severe consequences. Data and findings from the CIPHER team can help public health decision-makers be more forward-looking in the effort to contain H5N1.

“Through the large scale of high-performance and cloud computing, we employ AI and other modeling tools to answer such questions computationally. In this study, our aim is to be more forward-looking to predict the health impacts of H5N1 influenza before a major event catches us off guard.”
Colby Ford ’14,’15 M.S.,’18 Ph.D., CIPHER visiting scholar
Along with the earlier research published by eBioMedicine, a Lancet journal, the findings provide urgent insight as avian influenza poses an ongoing threat to global agricultural interests and raises increasing alarms for human health.
The team’s ability to model H5N1’s evolution in real-time measures how rapidly the virus can change, which is critical when it comes to anticipating and responding to public health threats.
“When you’re studying something as fast-evolving as a virus, speed is essential,” Janies explained. “Large data sets can be analyzed rapidly with high-performance computing and artificial intelligence to assess our preparedness for important problems such as H5N1 as it spreads to new regions and hosts, including American cattle and farmworkers.”
Janies and Ford, along with Bioinformatics Assistant Professor Richard Allen White III, Ph.D., led students Shirish Yasa, Khaled Obeid and Sayal Guirales-Medrano in the groundbreaking study, published after peer review in eBioMedicine on March 17.
At UNC Charlotte, faculty and student researchers have been analyzing protein interactions with avian and mammalian cell proteins for close to a year. Using computational tools assembled during the SARS-CoV-2 pandemic, the CIPHER team first published pre-print findings on H5N1 viral lineages in July 2024 — just four months after a farmworker in Texas was confirmed to have been infected by a cow and preceding a human death from H5N1 in Louisiana in December of the same year.
Via high-performance computational modeling, the team analyzed over 1,800 viral protein-host antibody interactions to track how H5N1’s hemagglutinin (HA) proteins — the key components the virus uses to enter host cells — have evolved. Findings suggest the virus is increasingly evasive of being bound by antibodies generated from previous infections or vaccinations, signaling a weakening of the immune response over time.
“High-performance computational modeling is a pathway for chipping away at multiple angles of biological variation at speed and scale,” Janies said. “It helps us tune our intuition to the right approaches for vaccine efficacy and infection control as viruses evolve.”
- “Predicting antibody and ACE2 affinity for SARS-CoV-2 BA.2.86 and JN.1 with in silico protein modeling and docking,” Frontiers in Virology
- “Predicting changes in neutralizing antibody activity for SARS-CoV-2 XBB.1.5 using in silico protein modeling,” Frontiers in Virology
- “Predictions of the SARS-CoV-2 Omicron Variant (B.1.1.529) Spike Protein Receptor-Binding Domain Structure and Neutralizing Antibody Interactions,” Frontiers in Virology
Anna Holt is a freelance writer based in Charlotte, North Carolina.